Why is this 866-470-6244 Phone Number grabbing attention? Anthem Blue Cross stands as a pillar in the U.S. healthcare system. This guide provides an in-depth look at Anthem’s services, explains the significance of its national contact, and helps you navigate the process of prior authorization. In this article, you will gain clear insights about 866-470-6244 benefits and procedures associated with Anthem Blue Cross.
866-470-6244 Overview
Anthem Blue Cross has served millions since 1944. It is known for its extensive network and dependable customer service. The table below offers a quick reference for key details:
| Aspect | Details |
|---|---|
| Founded | 1944 |
| Headquarters | Indianapolis, Indiana, USA |
| Coverage Area | Nationwide across the United States |
| Membership | Over 40 million members |
| Services Offered | Health insurance, prior authorization, claims support |
Introduction
Anthem Blue Cross is renowned for its expansive network and robust customer support. Accurate contact information is crucial when you need assistance with medical benefits. This article breaks down essential details and practical advice to help you navigate your healthcare options.
Reliable contact information like 866-470-6244 makes a difference when you require prompt service. Whether you need routine assistance or help with more complex processes like prior authorization, using official channels is key.
| Member Type | Contact Number | Purpose |
|---|---|---|
| National Members | 866-470-6244 | Prior Authorization and Support |
| Local Plan Members | (800) 274-7767 | Local Inquiries and Claim Status |
| CalPERS Members | (800) 451-6780 | Dedicated Support for CalPERS Members |
Background on Anthem Blue Cross
866-470-6244 Anthem Blue Cross has a long history of providing quality health care since 1944. The company has evolved to serve millions of members with diverse needs.
Legacy of Service
Anthem has built a strong reputation through decades of dedicated service. Its commitment to quality care is evident in every aspect of its operations.
Embracing Technology
The company invests heavily in digital platforms that simplify processes such as claims tracking and eligibility verification. These tools enhance the overall customer experience by reducing wait times and streamlining communications.
Nationwide Reach
Operating in all 50 states, Anthem ensures that every member has access to quality care. Its expansive network makes it a trusted provider across the country.
The Role of the National Hotline
For National members, the hotline 866-470-6244 connects you directly with a specialized team. This service handles inquiries related to prior authorization and other critical support needs.
Dedicated Support
When you contact the dedicated hotline, your inquiry is routed to professionals familiar with the specifics of your coverage. This personalized approach minimizes delays and errors in processing your requests.
Efficient Communication
The integration of digital tools with hotline support creates a seamless experience. Information is verified quickly, ensuring that your needs are addressed accurately.
Integrated Systems
Official digital platforms work alongside the hotline to confirm member eligibility and benefits. This system reduces complications and enhances overall efficiency.
Understanding the Prior Authorization Process
Prior authorization is a key process that confirms whether a service meets the guidelines for coverage. It ensures that only medically necessary procedures are approved, protecting you from unexpected costs.
What Prior Authorization Entails
Prior authorization involves a thorough review of your medical service request. Your provider submits detailed documentation, including your medical history and member details, to confirm that the proposed service is appropriate and covered.
The Process Explained
Initiation of Request
Your provider starts the process by submitting a detailed request. This submission includes all pertinent medical and personal information.
Verification of Details
Digital tools verify your eligibility and confirm that the information provided is accurate. This step is crucial for a smooth process.
Clinical Review
A review by Anthem’s Utilization Management team follows. Experts assess the request against established clinical guidelines to determine its necessity.
Final Decision
After review, you receive a decision. If approved, the service is scheduled, and your provider is notified; if denied, you receive an explanation along with next steps.
The table below summarizes the process:
| Stage | Action Taken | Tools Used |
|---|---|---|
| Initiation | Provider submits the request | Provider portal, phone call |
| Verification | Member details are confirmed | Digital verification tools |
| Clinical Review | Request is assessed for medical necessity | Utilization Management team |
| Final Decision | Approval or denial is communicated | Notification via digital tools |
Real-World Use Cases

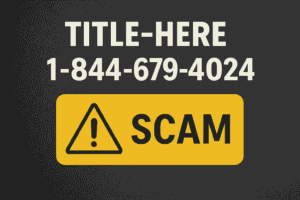
866-470-6244 Phone Number presented with a high-tech design.
Real-life scenarios highlight how the prior authorization process benefits members. These examples illustrate how clear communication leads to efficient service delivery.
Medical Referrals
When a specialist referral is needed for a chronic condition, your provider initiates a request. This process ensures that the referral is approved quickly, minimizing delays in receiving care.
Elective Surgical Procedures
Before an elective surgery, your provider submits a request to verify that the procedure is medically necessary. This step protects you from unexpected costs by confirming that the surgery is covered by your plan.
Prescription Medications
Some medications require approval to be covered. In these cases, your provider submits the required documentation, ensuring that you are not burdened with high out-of-pocket expenses.
Each scenario demonstrates that efficient documentation and clear communication lead to faster approvals and improved care outcomes.
Verification and Authenticity
Verifying contact information is essential in today’s digital age. Always use official channels to confirm that you have the correct details.
Cross-Reference Official Sources
The Anthem Blue Cross website and your member ID card are reliable resources. Digital tools such as secure portals provide up-to-date contact details, ensuring you use the correct numbers.
Secure Communication
Using verified channels protects your personal and medical information from fraudulent activities. If you receive an unsolicited call, verify its authenticity before sharing any details.
Protecting Your Information
Taking simple steps to verify contact information can save you from potential scams. Trust only official sources to safeguard your data.
Additional Contact Information
Anthem Blue Cross provides various contact numbers to cater to the diverse needs of its members. It is crucial to use the correct number for your specific situation.
National vs. Local Support
National members have access to a specialized hotline that handles complex requests efficiently. Local Plan members and CalPERS members receive dedicated support tailored to their specific requirements.
Confirming Your Contact
Always refer to the contact details on your member ID card. Verification through official websites ensures that your inquiry is directed to the correct department.
Steps for Confirmation
Before making any calls, check the official Anthem Blue Cross website. This practice minimizes miscommunication and prevents potential delays in service.
Frequently Asked Questions
This section addresses common questions regarding Anthem Blue Cross and the prior authorization process.
What Is Prior Authorization?
Prior authorization is a review process to determine whether a requested service meets clinical guidelines. It ensures that the service is covered under your plan.
When Should I Request Authorization?
You should contact your provider when a service or medication requires prior approval. Have your member ID and relevant medical documents ready to expedite the process.
How Can I Verify Contact Details?
Verify contact information using the official Anthem Blue Cross website or by checking your member ID card. Digital tools offer an additional layer of confirmation.
What If I Suspect a Fraudulent Call?
Do not share personal information if you suspect a call is fraudulent. Before proceeding, use official channels to confirm the authenticity of the call.
Conclusion
866-470-6244 Anthem Blue Cross is dedicated to providing efficient, accessible support for its members. The combination of dedicated hotlines and advanced digital tools ensures that every inquiry is handled accurately and promptly. By understanding the prior authorization process and verifying contact details through official sources, you can manage your health care benefits with confidence.
Accurate information and clear communication are critical to receiving timely care. Following the guidelines in this article will help you avoid unnecessary delays and ensure that your medical requests are processed smoothly.
Your proactive approach to verifying details and using the correct channels enhances your overall health care experience. For any urgent questions or to confirm coverage details, always refer to the official resources provided by Anthem Blue Cross.